Nature Medicine reports that a federally funded Phase II trial at the Abramson Cancer Center and Perelman School of Medicine at the University of Pennsylvania has, for the first time, enabled clinicians to detect dormant breast cancer cells in survivors and eradicate them with FDA-approved drugs.
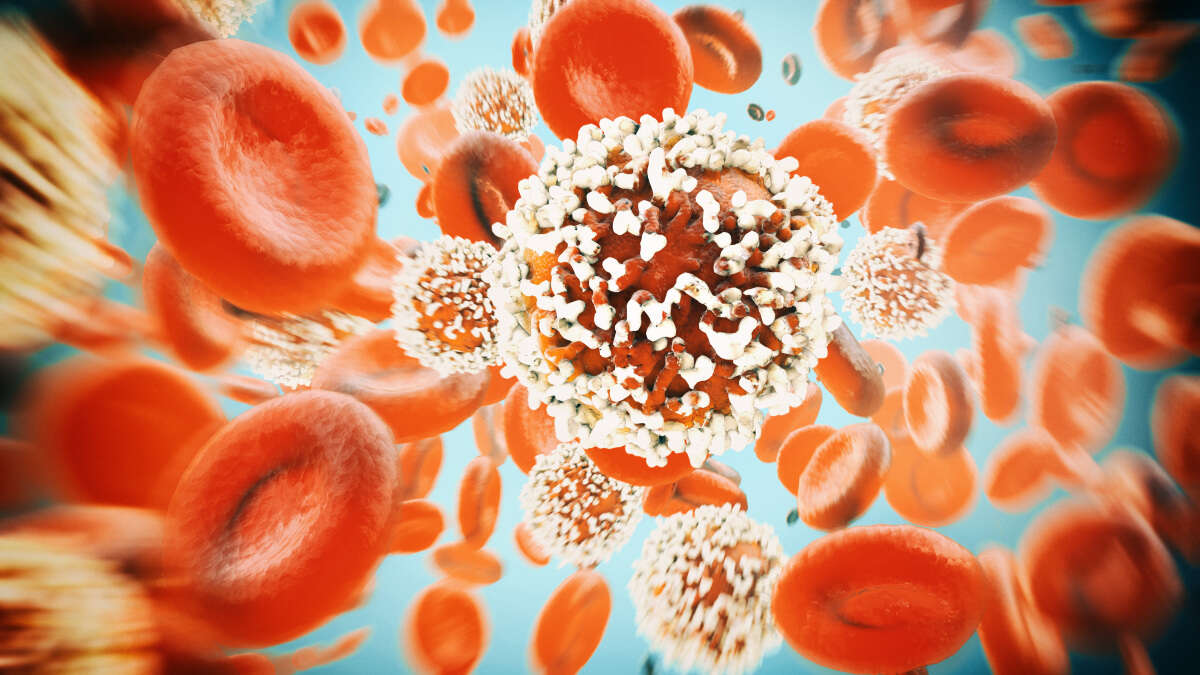
Nature Medicine explains that, despite improved survival through early detection and treatment, breast cancer recurrence remains incurable for about 30% of patients, including triple-negative and HER2-positive tumors that recur within years and estrogen receptor-positive cancers that can reemerge decades later. Until now, no strategy existed to identify survivors harboring minimal residual disease or to intervene preemptively.
Nature Medicine details a randomized Phase II study of 51 survivors screened for dormant cells. Positive cases were randomized to receive one of two monotherapies or both drugs. After six to 12 months of treatment, 80% of those on single agents and 100% of those on combined therapy had no detectable sleeper cells. Three-year relapse-free survival exceeded 90% with monotherapy and reached 100% with combination treatment.
Mariann T. and Robert J. MacDonald Professor in Breast Cancer Research Angela DeMichele, the study's principal investigator, said "The lingering fear of cancer returning is something that hangs over many breast cancer survivors after they celebrate the end of treatment" and noted that targeting dormant cells represents a promising preventive approach.
Lewis Chodosh, chair of Cancer Biology, said, "Our research shows that this sleeper phase represents an opportunity to intervene and eradicate the dormant tumor cells before they have the chance to come back as aggressive, metastatic disease" highlighting the distinct biology of dormant versus active cancer cells.
Preclinical mouse studies by Chodosh's team demonstrated that two FDA-approved drugs interfering with autophagy and mTOR signaling effectively cleared minimal residual disease, prolonging remission.
DeMichele's group screened survivors treated within the past five years who had clear scans, enrolling those with sleeper cells into the CLEVER trial. Patients received six cycles of monotherapy or combination therapy. With a median follow-up of 42 months, only two participants have relapsed.
DeMichele said "We want to be able to give patients a better option than 'wait and see' after they complete breast cancer treatment" underscoring the team's optimism.




